Overview of Horse Digestion and G.I. Tract Anatomy
Updated April 14, 2025
Digestion is the process of breaking down food and absorbing nutrients. Each part of the horse’s digestive system serves a different purpose, and each area has unique health concerns.
Basic Anatomy of the Horse GI Tract

The equine gastrointestinal tract can be divided into two main sections:
- Foregut – consists of the mouth, esophagus, stomach and small intestine.
- Hindgut – consists of the cecum, large colon, small colon, and rectum.
Stomach
The horse only has one stomach and it is only able to hold 3-5 gallons at a time, making it relatively small compared to body size. Depending on how big the meal is and what it contains (e.g., hay vs. grain vs. liquid) food may remain in the stomach as little as 15-30 minutes or as long as 12 hours, with 3-4 hours being average.
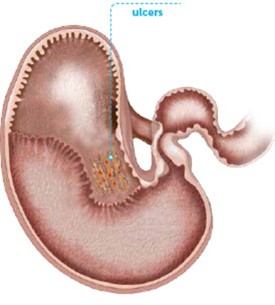
Dubbed the “non-glandular region,” the upper 1/3 or so of the horse's stomach is where 80% of ulcers form since this area does not have protection from acid like the lower, glandular portion does.
Small Intestine
The next part of the horse's digestive tract is the small intestine. Approximately 70 feet in length, it is made up of three parts:
- Duodenum
- Jejunum
- Ileum
Food moves through the entire small intestine in as little as 30-60 minutes but can take longer (up to 8 hours).
Large Intestine
Continuing to the large intestine, the small intestine empties into the horse's cecum. Basically a fermentation vat (similar to the rumen of a cow), this comma-shaped structure on the right side of the horse is approximately 4 feet long and holds 8 gallons.
From the cecum the order is the large colon (10-12 feet long), then the small colon (also 10-12 feet long) then the rectum (about 1 foot long). Time for passage through the whole hindgut can range from less than 1 day to as many as 3 days.
The Equine Digestive Process

Since the functions carried out in the front of the horses GI tract versus those carried out in the back of the GI tract are very different, we will focus on each part separately.
Foregut Digestion
After food is gathered up, chewed, and swallowed, the stomach kicks into gear. The main functions of the horse's stomach are to:
- add gastric acid to help with the breakdown of food
- secrete the enzyme pepsinogen to begin protein digestion
- regulate the passage of food into the small intestine.
The stomach is a holding and mixing tank, not unlike a cement truck that is constantly churning and mixing ingredients.
While food breakdown may begin in the stomach, it continues in the small intestine, where secretions help with the further digestion of protein, simple carbohydrates, and fat. The small intestine is also the main site of nutrient absorption once they are in small enough form. Amino acids, glucose, vitamins, minerals, and fatty acids are taken into the body as they move along the small intestine, so progress shouldn’t be too fast or too slow.
Hindgut Digestion
Horses are hindgut fermenters, which means the bulk of digestion happens in the large intestine. The processes that occur in the cecum and colon are less about breaking down food into smaller, absorbable particles with the aid of enzymes and more about fermenting complex carbohydrates (fiber) into useful end products. Complex or structural carbohydrates includes forage (hay, pasture, etc.) which makes up the bulk of your horse’s diet.
In this stage, probiotics (known as “good bugs”) assist in the digestive process. In addition to generating volatile fatty acids, which supply energy or calories, these helpful microorganisms that make up the horse’s microbiome, also produce B-vitamins, Vitamin K, and some amino acids.
The colon then serves not only to absorb these nutrients, but also a portion of the water that accompanies food as it moves along the last portion of the digestive tract. This is where fecal balls are formed before exiting the GI tract.
Problems Within the GI Tract
With all these moving parts, it’s no wonder sometimes things don’t always run smoothly. However, just because the GI tract of the horse is long and complicated shouldn’t keep owners from doing their part to help maintain a healthy digestive system.
To understand where best to focus these efforts, it’s important to understand the most common problems of the foregut (gastric ulcers) and the hindgut (colic). To learn about these GI conditions including their clinical signs, treatments, and tips for prevention, go to each article linked below:
While owners can take steps to prevent occasional digestive upset, working with your veterinarian to ensure your horse is being managed and fed appropriately may reduce his risk level. One approach your vet may recommend is daily support from a supplement to help your horse cope with digestive stress.
Supplements to Support Healthy Digestion

A combination effort of daily support from a digestive supplement and smart management practices can help ensure your horse has what he needs for a healthy stomach. Ingredients to look for in a digestive supplement for your horse include:
- Calcium and magnesium - helps neutralize gastric acid
- Glutamine – helps repair intestinal tissue
- Glycine – inhibits gastric secretions to protect the stomach lining against chemical and stress induced lesions (ulcers)
- Soothing herbs like licorice root and aloe vera
- Probiotics – play a key role in the digestive process
- Prebiotics - have been shown to reduce disruption in the hindgut
- Yeast - can improve fiber digestion and assist in adjusting to feed changes
- Enzymes - have been shown to increase proper digestion of starch in the foregut
Additional Horse Owner Resources and References
- Visit our guide on equine nutrition to understand more about forage, grain, vitamins, and minerals that make up your horse’s diet.
- Learn about the benefits of probiotics and prebiotics.
- Enroll your horse in ColiCare, our free program that provides up to $15,000 in colic surgery reimbursement.
- Read Equine Applied and Clinical Nutrition by Raymond Geor, Pat Harris, and Manfred Coenen.
Horses will be horses, and no feeding or management system can fully prevent the accidents and injuries or disorders and conditions they are prone to. But gaining a better appreciation for what’s normal and not-so-normal when it comes to the elegant, yet fragile digestive system of the horse can still make a big difference!